The proposed changes to the Mental Health care system have been launched to much acclaim from both the media and certain sections of the mental health community. However, the announcement is light on details and demands scrutiny from the media and the general public. Aaron has outlined the known facts of the proposed reform as well as listing some key questions that need answers.
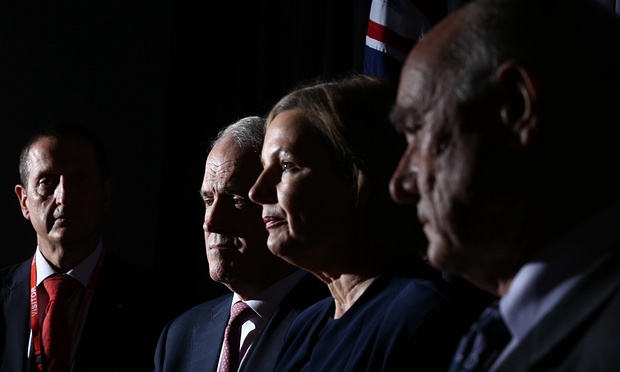
Last week, amid much fanfare, Prime Minister Malcolm Turnbull and Health Minister Sussan Ley were joined by Mental Health expert Professor Ian Hickie and Mental Health Commissioner Professor Allan Fels, in order to launch a sweeping round of changes that would revitalise the mental health sector and begin to address what has been described as a “hopelessly fragmented system”.
I have been meaning to post about these new changes for about a week now. However, the lack of detail presented in the available documents has made it difficult to determine exactly what the changes being proposed are. I am curious that organisations such as Beyond Blue and The Australian Psychological Society among others were front and center with their praise for changes about which very little is known. The Australian Medical Association, and the Australian and New Zealand College of Psychiatry were far more reserved in their assessment of the package, demanding more details from the government.
So I thought what might be useful is to consider what we actually know, and what can be surmised by reading between the lines.
Fact 1 – There is no new money in the reforms proposed
Despite the mental health sector being universally recognised by health economists as having about half the money that is required to provide optimal service, and despite Mr Turnbull’s appeal to the economic benefits of good mental health care in his launch, there is no new money. Therefore, any new proposals need to be considered both in terms of what they offer, but also what is being taken away in order to fund them.
Fact 2 – Patients with “Mild” mental heath conditions will be offered online therapy
This online therapy will be offered as a first line of treatment instead of face to face therapy. On the face of it this is excellent policy. Online therapies get similar outcomes compared with face to face, and of course once the computer programmers have finished writing the thing, it runs virtually cost free other than hosting a bit of server space and some bandwidth. There are a few problems with online therapies that haven’t been mentioned in any of the policy documents. They are as follows:
- Despite getting excellent outcomes for those who complete online therapy courses, most people don’t complete. The most recent figures I saw, suggested that as many as 90% who start online therapy courses never come back to complete a second session. This recent study published in the British Medical Journal, found that online therapies actually offer no benefit to patients over and above standard GP care.
- The idea that “Mild” mental health conditions exist as a discreet category is a fallacy that could only be put forward by someone who is completely ignorant of mental illness. Find me the most severely unwell person in any psychiatric facility you care to name, and I will show you someone whose mental health problems were once mild. The Australian Government has been leading the charge towards early intervention and prevention for almost two decades now. It seems like a very mixed message to suddenly say that there are some people whose problems aren’t serious enough to deserve treatment. Does the government plan on achieving cost savings by also suggesting that some cancers are not serious enough to treat yet ?
Fact 3 – New programs will be run through the existing Primary Health Networks
The government plans to invest around $350 million into helping people at the severe end of the spectrum by channelling money toward regional “Primary Health Networks” (PHN) so that they can then purchase integrated care packages that best suit the person. Again, this is a wonderful aim. the needs of people with severe mental illness have always been grossly neglected in this country. Integrated care seems like a worthwhile goal, until you look at it in a bit more detail.
- The Primary Health Networks exist because Medicare Locals were deemed to be massively inefficient in terms of their use of funds. There is no suggestion of fraud or incompetence here, just the simple reality that if you give an organisation a pot of money and then ask them to lease premises, appoint a high 6 figure salaried CEO, a number of low 6 figure salaried executive officers, produce marketing material, networking dinners, websites and all of the other bureaucracy required, only a certain amount of the funding trickles down into actual service delivery. The new Primary Health Networks are basically the same model as the old Medicare Locals, there are just a few less of them. The PHNs do not deliver services themselves, they don’t employ doctors and nurses, psychologists and mental health clinicians (actually they do, but most are employed as policy officers, trainers or researchers), they will contract out the services to others through tender.
- Tendering of services is supposed to be the most efficient way of delivering services, because all service providers compete to offer the best service at the lowest price. In reality, tenders are often won by organisations that employ excellent tender writers. They employ excellent tender writers with the profits they make from winning profitable tenders. They make these profits, by charging high prices to the person with the money, and then paying low wages to the people delivering the services.
- The most likely outcome of this model of care is that a lower quality of mental health care will be delivered by less qualified staff at a greater cost to the taxpayer.
Fact 4 – We have no idea which programs are being de-funded
The money has to come from somewhere. The government is virtually silent on which services will be cut in order to fund the new initiatives. However, the report from the mental health commission that the current reforms are based upon is pretty clear. Some of the money will come from cuts to funding hospitals, and some of it will come from cuts to funding for private psychological services through medicare (The Better Access Initiative).
- Whenever I enter a public or private psychiatric facility, I never feel like I am walking into a place of opulence that is clearly over funded. Every Coronial report that I read into a suicide, homocide or police shooting seems to have a whole section devoted to the failures of the hospital based mental health system, and this section nearly always concludes that the staff in these organisations are doing the best they can with the resources they have got, before pointing the finger squarely at government to give them more resources. I am not prone to hyperbole, but I strongly believe that cutting ANY funding front he public mental health system will lead to an increase in completed suicides.
- The “Better Access” program has been in place for 9 years now and has been providing publicly subsidised allied health (but mostly psychology) services to those people whose GPs felt would benefit from them. This program has drawn criticism from a range of sectors for being an over-funded arm of middle class welfare. However, independent evaluations have never supported the critics of this program. Better Access provides services cheaply for the government, has lead to an almost doubling of the percentage of the population who are accessing psychological care, and produces excellent outcomes. These facts have not deterred the program’s critics, rather they have just begun repeating the same criticisms in more media outlets with the hope that the criticism will simply outweigh the facts in the public consciousness. Cutting funding from Better Access will reduce the percentage of people accessing high quality mental health care, putting more pressure on public hospitals at the same time their funding is also being slashed.
Evaluation
Again, without clear statements from Minister Ley, It is difficult to accurately evaluate the impact of the proposed changes. However, the uncritical acceptance of these changes by the mental health community it both naive and demonstrates an incredibly short memory. I have now lived through too many health minsters, mental health ministers, five year plans, reforms, restructures and rebrandings to have anything but cynicism toward the motives of government. I do not have any faith in our elected representatives to act in the best interests of mental health consumers unless they are afraid of losing their jobs. If you care deeply about mental health issues, then contact your local MP and demand that they answer the following questions.
- For all of the talk of improved outcomes in the mental heath sector, why is not one dollar of additional funding being proposed ?
- Which programs are you planning on defunding and by how much ?
- Where is the data that demonstrates that the proposed changes will lead to better outcomes for people with mental health conditions
- How will the proposed changes be evaluated
A lawyer friend once told me that mental health will never get a fair go in Australia because those who are severely affected are too unwell to stand up for themselves. What is being promised by the government right now is “Once in a generation change”, it is up to all of us to stand up and demand answers to these questions from our government as to how they plan to do it.
As a consumer I resent the fact that people who suffer with depression and anxiety illness are deemed as having a “mild” mental health issues when statistics clearly show an overwhelming majority of suicides in this country are attributed to these illnesses, recovery is always in flux and a life long battle to keep these type of illnesses at bay.
These changes WILL COST LIVES!!!
All mental health issues need to be recognized, treated and supported equally.
I Could not agree more Louise. Mental Illness is not a category, it is a spectrum. Best practice is to provide help as soon as possible rather than to wait until it deteriorates.
Hanks for the article Aaron. As a clinical psychologist, in private practice, we provided most of our services under the Better Access Scheme through a Mentsl Health Care Plan. We charge a gap but bulk bill those on low income or health care cards. Our gap is quite modest and even those who pay often struggle to find the $45 for their fortnightly sessions. The fallacy that this scheme is welfare for the Middle classes is only used by politicians and critics of the system who have never had to juggle the expenses of living a middle class life! We charge a gap, because the research shows that people invest more in their own recovery if they have a financial investment in their treatment, we don’t charge a gap to “make money”.
Our practice goes above and beyond for our patients on a daily basis. We advocate for them to NGO’s and government run health institutions, to try to get them extra help, but there is rarely places for them. These patients would be on the “mild to moderate” but these are the same people who like others have commented upon are likely to complete a suicide or at least attempt it. The hidden expenses on the health system, the legal system, the families is never reported when this type of costing is discussed.
The federal and State governments actually cannot afford to cut funding to private Psychologists, for if they do there will be a pandemic of people presenting to ED’s for treatment that we used to provide to them. Maybe then they will wake up and realise that throwing money at NGO’s and creating PHN’s who only make MH work more difficult not easier is not the answer.
Finally, it astounds me and makes me angry that getting a Medicare rebate for accessing a private psychologist or other allied healthcare provider is limited to 10 sessions. This is the only health issue that has a limit to access for helping manage the illness or to recover from an illness. If a person has diabetes, asthma or hepatitis (all potentially life threatening illnesses if left untreated), the health authorities would never consider limiting the amount of times they could access help to help the patient manage their illness. Mental health issues, depression, anxiety, borderline personality disorder (hugely prevalent in the community) and other MH issues such as PTSD all have a huge risk of the sufferer attempting or completing suicide, but the impact on their family is also significant. We need much more money invested in MH not just “rearranging the deck chairs on the Titanic”.
Very well done Aaron. I’m glad to see someone with insight looking at the reforms with a first-hand fine tooth comb. Brilliant questions at the end. Thank you.
I very rarely put my two-bobs worth in when it comes to politics,but quite frankly I’m at the end of my tether.So here goes.I am a very,mature age student in the third year of a Bachelor of Psychological Science.I am working very hard to get the marks to do Honors.Honors are required for Registration,with two years extra under Supervision;i.e. six years in total.I have worked in Mental Health related welfare positions and have been in Management in other areas.I was always very confident and sure of myself.I had enjoyed good Mental Health most of my life until a few years back when circumstances in my life changed dramatically.As a consequence,I suffered with Major Depression/Anxiety.Believe me it is not a mild, nor a moderate condition.If I had been diagnosed early and treated,I’m convinced I would not have suffered to the point of suicidal ideation.
However,I was very lucky finding a switched on GP who put me under a Mental Health Care Plan,and through the Better Access Scheme I chose my own Counseling Psychologist.If I had not had that opportunity for this type of care I would probably be quite a burden for government in being possibly unemployable up until my retirement,and beyond.That is,if I wasn’t very dead through the pull of the black dog.
The type of narrow,short-sighed decisions being forwarded by government would cost all of us(present/future)a lot more in social/health costs.As it stands now I have great empathy for sufferers of poor Mental Health.I was fortunate enough to receive the help I needed.Others who could under the current arrangement have the same opportunity as me, may not be so lucky,and as a result may become a great burden on loved ones, government and personally go through years of enormous suffering and despair.
The previous government put the retirement age for my age group to 68 years.I had hoped to finish my working life helping others as a professional clinician, coming from my personal experience and my training.This possibility is now looking somewhat less possible.I will however,find a way to achieve my goals in helping others, no matter what.It does make me reconsider putting in more time at present though to do Honors as it will increase my HECS debt,take a lot more time to finish and may be an exercise in futility as it is getting pretty competitive out there. Maybe, I could go bush.I only mention this to point out some other possible roll-on effects of the government’s possible actions.
The government may well say that these types of decisions are pragmatic.I will posit that they are politically expedient, lazy,ideologically driven,and uncaring decisions.If these types of funding cuts go ahead it will have a devastating psychological/sociological affect on our country in the long-term.Blind Freddy can see that!If it is correct that the APS is in support of these funding decisions,where on the good earth are we heading!
When will these bureaucrats and politicians learn to look at issues from a balanced socioeconomic perspective.When will they learn that most thinking Australians are over their outdated ideologies.These types of decisions are driven more by a corporate, Neo-Conservative ideology than really caring about your people and the health,harmony,well-being,and benefit of the society.This neo-con thinking is reflective of a slight of hand undercurrent of further globalising through removing sovereignty of future governments by means of such surreptitious agreements as the TTP.Whatever happened to transparency of governance?
The Liberal/Nationals have been trying to slowly dismantle Medibank/Medicare since getting Whitlam out.While I’m on that point, how do you distinguish oral care from the rest?
I am not a member of any political party but I feel we need a groundswell scheme to weed out these types of narcissistic people from government,and replace them with humanitarian thinkers of higher cognitive prowess and conscience who will manage the country for the benefit of all of the people, not just those in the big end of town.If they make promises at election time make them write it as a legal contract that carry penalties for breach.
Will we ever have a free market economy with a social conscience,as opposed to a capitalist dog eat dog mentality that we are now moving closer and closer toward?I remember Hawke bashing on ad nauseam about how he wanted to follow the Swedish political model.Whatever happened to that? Oh, that’s right when his mate Keating was PM he then sold off the Commonwealth bank.The people’s bank set up in 1938 by the Labor government. The bank that never charged administration fees or other such greedy nonsense and was still profitable.Oh,maybe it was to allow foreign banks to do as they pleased and charge like wounded bulls.OK,I let off a little steam but maybe we should import some politicians from Denmark.They still have free university,free schooling,great health care and consider your teeth as part of your body.